Over 17,000 children in NI waiting over 1 Year on 1st Consultant Appointment

“The report presents a concerning picture of the number and length of waits for services, this includes red flagged first consultant out-patient appointments[i] which are either confirmed or suspected cancers where we found that 24 children were waiting over 1 year”.
The Review examined the number of children and young people on waiting lists, and the length of time they wait to access first or review appointments with consultants, for treatment in hospitals, and for community-based services, it also assessed the impact that waiting has on children and young people and their families.
Koulla said, “While the impact of waiting on a red flag or urgent[ii] appointment is clear, we know that delayed access to any specialist support, whether that be for autism diagnosis or support, CAMHS, physiotherapy or speech and language, can and does have a profound impact on a child’s health outcomes, emotional and mental wellbeing, educational attainment, relationships with family and friends and quality of life more broadly.”
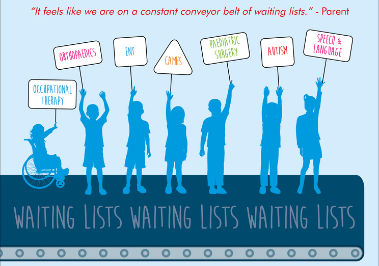
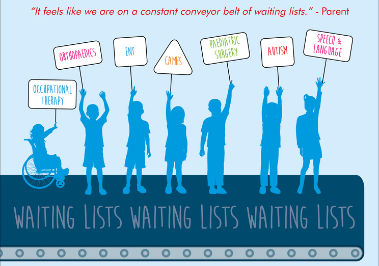
“The stress and pressure on parents and carers as advocates for their child, experiencing delays in accessing healthcare is significant. A clear message from them was that communication, co-ordination and emotional and practical support is inadequate and needs to be improved. These are the most basic expectations of these services and are particularly important when waiting times are as long as they are. Therefore, I have recommended an interim regional waiting list management process for child health services be established while overall reform is on-going.”
The Review highlights that, 1 in 5[iii] children and young people in NI are waiting for a first or review outpatient appointment with a consultant. It also found that 17,194 children and young people were waiting over 1 year and 510 over 4 years for a first consultant out-patient appointment. (See infographic in notes to editors for full infographic)
1 in every 47 children in NI with conditions that require surgery or procedure are waiting for an in-patient or day case appointment. In April 2021, 62% (6092) were waiting over 1 year, and 197 over 4 years.
Koulla continued “While these hospital care statistics are shocking at least we get a clear picture. Worryingly, we have found a complete absence of regional monitoring or reporting of waiting times for community child health services which makes it impossible to get a clear understanding of the number of children waiting for these services[iv]. This review found that at least 26,818 (1 in 16) children in NI are waiting for a community-based health service and that figure is likely to be much higher given the limited data that was available.”
Community Child Health Services include Speech and Language, Occupational Therapy, Physiotherapy and Podiatry.
Koulla explained, “Some families are travelling internationally to access time-critical health treatment, such as surgery for scoliosis, due to the extent of delays in the Northern Ireland health and social care system[v]. At the same time, we have the number of children waiting for an assessment for autism increasing by 148% in 5 years with a 687% increase in the number waiting more than 1 year for an assessment[vi]– it is a system where capacity in nowhere near meeting demand.”
The Review highlighted that there are three times more paediatric posts vacant for over 3 months in Northern Ireland compared to England, with workforce provision in rural areas a particular problem.[vii]
Koulla Continued, “It is also deeply frustrating that there has been no official progress update report published for the ‘Strategy for Paediatric Healthcare Services Provided in Hospitals and in the Community in Northern Ireland 2016-2026’. Our Review has found that only some limited transformation funding to progress actions from the Strategy was made available in 2019 – three years after the Strategy was first published.”
The Commissioner concluded, “More Than A Number makes 17 recommendations[viii], these include a full review of the child health system to ensure that health and social care reform is based on an up-to-date understanding of need across the system, takes account of existing plans for the reform of children’s health services but also identifies where the gaps are. I am also calling for improvements in the visibility of, and accountability for, children’s health within key departments by ensuring that key high level dedicated posts are in place to oversee commissioning, policy and service delivery. One of which is the appointment of a Deputy Chief Medical Officer for Child Health.[ix]
“The commitments given by the current Health Minister to improve waiting lists and address the underlying issues which drive them is very welcome. It is important that the scope of the work is broad enough to cover all child health services.
“Waiting times are one of the clearest indicators of a system under immense strain and unable to meet the needs of its population. We must strive to get to a point where all children and young people can get access to the right care, at the right time and in the right place and that no child is left waiting months or years in a queue to access services. Children have a right to receive high quality care without any unnecessary delay.”
The Commissioner committed to monitoring the implementation of the recommendations in this Review and will publish a progress update report in Autumn 2022, before the end of her Term as Children’s Commissioner.
ENDS
Notes to Editors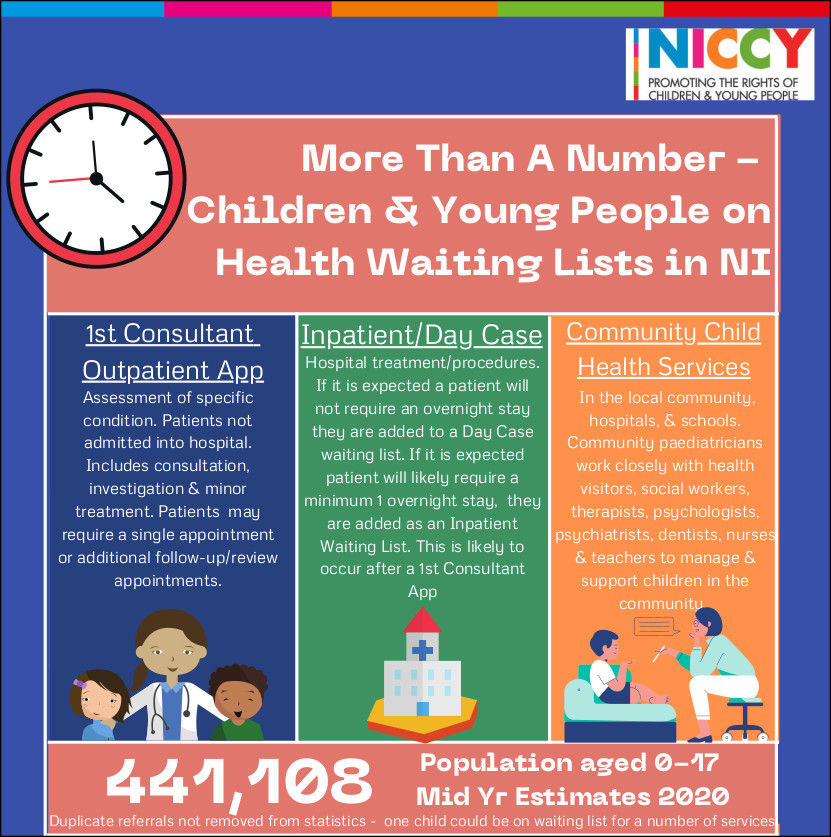
[i] These include consultations, investigations & minor treatment of specific conditions where patients are not admitted into hospital.
[ii] Urgent – (requiring urgent attention appointment, surgery or tests)
[iii] August 2021
[iv] Community Child Health Services take place in the local community, hospitals, & schools. Community paediatricians work closely with health visitors, social workers, therapists, psychologists, psychiatrists, dentists, nurses & teachers to manage & support children in the community. They include services for Speech and Language Therapy, Occupational Therapy Services, Orthoptics Service, Nutrition and Dietetics, Physiotherapy and Podiatry. There is no regional monitoring and reporting of waiting times for community child health services (apart from Autism diagnosis and intervention and CAMHS) and individually HSCTs only monitor waiting times for some services.
[v] A 2019 Freedom of Information request from local charity ‘Megan’s Wish’, revealed, 311 children were diagnosed with scoliosis in Northern Ireland that year. At June 2020, 31 children were waiting for fusion surgery with an average wait of 36 wks for an urgent referral and 43 wks for a routine referral. International best practice for this type of surgery is 16 weeks. It is estimated that in the last three years, ten children and young people have travelled to Turkey to undergo privately funded ‘time critical’ surgery because it could not be provided by the NI HSC system within the time frame needed.
[vi] Autism NI – Number of children waiting for an assessment for autism increased by 148% in 5 years between 2016-2021 (2079 to 5155), with a 687% increase in the number waiting more than 1 year for an assessment (279 to 2195).
[vii] Workforce Census: Focus on Northern Ireland (2019) – RCPCH
[viii] Recommendations from the review include a range of enabling structures and process that include: A full review of the child health system, collection and monitoring of a greater depth of information regarding patient experiences and outcomes, appointing a Deputy Chief Medical Officer for Child Health. Appointing a policy lead for child health at the Department of Health to oversee the planning and delivery of child health services across the health and social care system and establishing a single point of entry process across all HSCTs for all child health services. Further strengthening of collaboration with neighbouring jurisdictions in the delivery of health services for children, improvements in performance management and waiting time measurement and reporting.
[ix] Outstanding recommendation from the 2018 report of the Inquiry into Hyponatremia related deaths in NI.